Best Practices For Optimal Stomach Acid & Digestion
Sometimes bloating, belching or heartburn after a meal is nothing but a fleeting irritation, but all too often it becomes a chronic problem. When patients feel overly full, develop severe heartburn, continually bloat or belch, or their doctor diagnoses them with gastrointestinal disease, something is clearly amiss.
The Digestive System & Immunity
Studies indicate 70% of immune cells reside in gut-associated lymphoid tissue. This tissue also has 80% of plasma cells responsible for producing antibody molecules which attack antigens; toxins or other foreign substances that induce an immune response. This is why I stress the importance of a properly balanced, healthy digestive system – it improves overall health!
When your digestive system does not work properly, it can cause nutrient imbalances and deficiencies. It can also cause a microbial imbalance in the gut or adapt to cause more harm than good.
Not surprisingly, many studies show impaired microbiota can cause diseases and health problems as it affects your immune system. Studies suggest it plays a role in inflammatory bowel diseases, obesity, diabetes, liver diseases, chronic heart diseases, cancers, HIV, and autism.
Unfortunately, restoring health by nurturing the digestive tract is not widely understood or practiced in conventional medicine. Instead, doctors learn to suppress symptoms, usually by blocking the production of stomach acid.
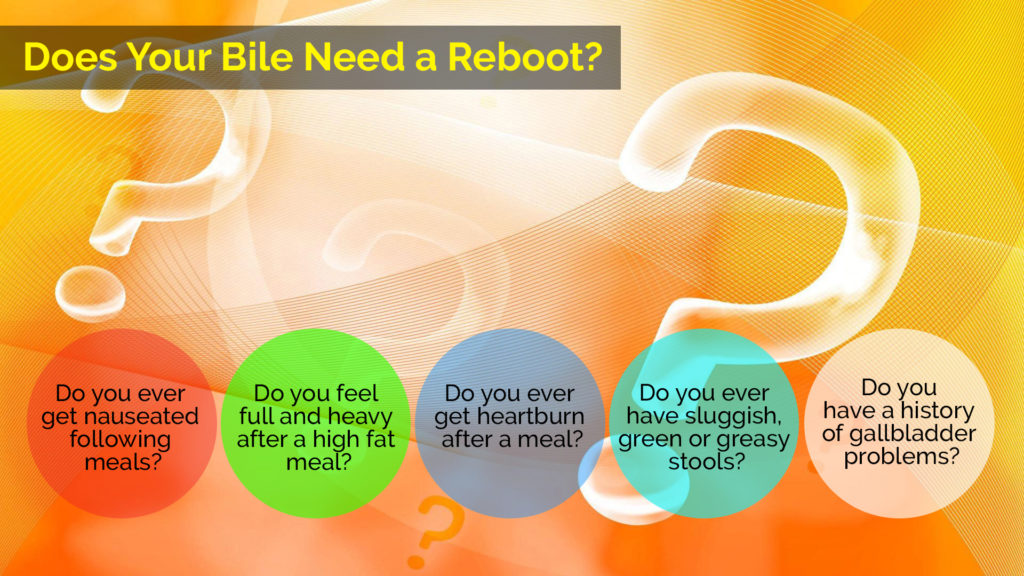
The Importance of Stomach Acid
Taking an antacid to alleviate heartburn or an upset stomach may seem a logical choice, but reducing stomach acid levels actually causes additional problems. Stomach acid serves many important purposes.
Sterilizes Food & Drink
When you consume food or drink you may unintentionally consume harmful bacteria and microorganisms too. Some organisms can survive high heat from cooking and even pasteurization. Stomach acid is one of your body’s first defenses to neutralize pathogens.
Breaks Down Protein
Protein is the hardest food category to digest, because it has long, strong chains. To digest it well, you need sufficient stomach acid and other digestive juices.
Activates Pepsin Enzyme
Stomach acid activates pepsin, necessary to metabolize protein.
Activates Intrinsic Factor
Stomach acid also activates intrinsic factor, a protein that helps your body absorb vitamin B12.
Stimulates Bile & Enzyme Release
Bile assists in the digestion and absorption of fats and fat-soluble vitamins and the elimination of waste. Pancreatic enzymes assist in the digestion of fat, carbohydrates and proteins.
Protects Esophagus
Stomach acid triggers the closure of the esophageal sphincter to protect the esophagus from acid damage.
Triggers Food Movement
Stomach acid also triggers the pyloric sphincter which moves food from the stomach to the small intestine.
Low stomach acid levels can create a vicious, unhealthy cycle. You do not digest food well, which can lead to chronic inflammation in the gut, leaky gut syndrome, microbial overgrowth, less nutrient absorption, and elevated stress hormones. These lead to further health issues.
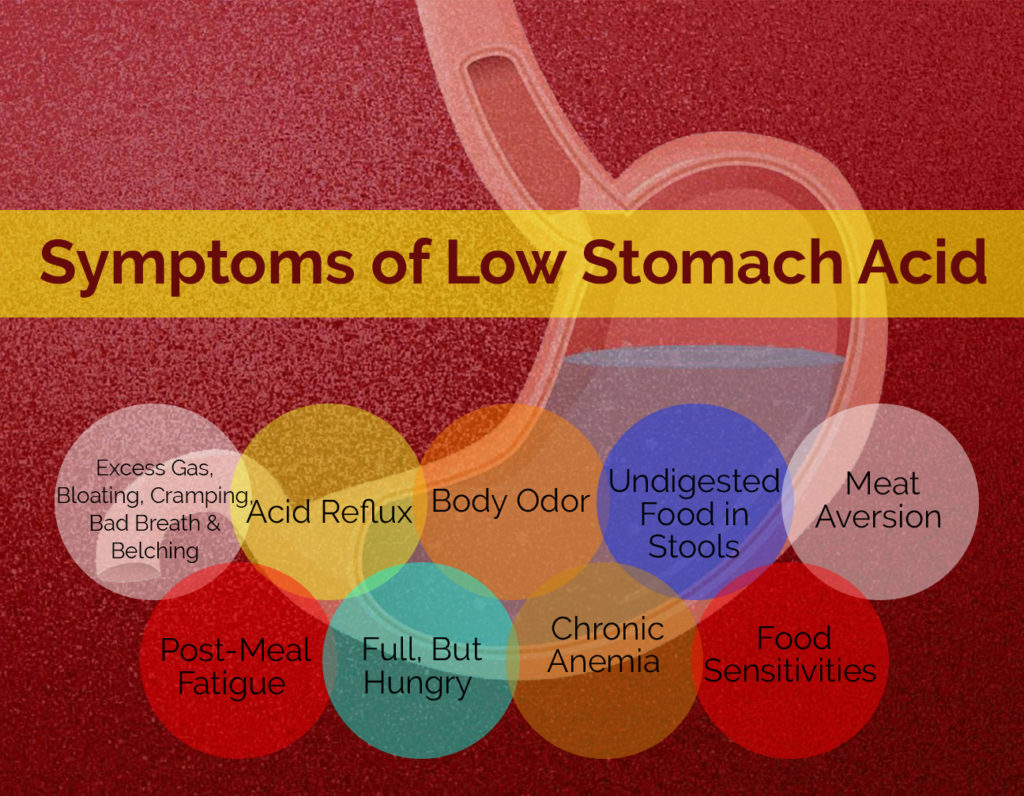
Symptoms of Low Stomach Acid
Ironically, the conventional treatment for many of these symptoms is acid-suppressing medications, instead of increasing it.
Excess Gas, Bloating, Cramping, Bad Breath & Belching – usually within an hour after eating due to bacterial fermentation in the stomach
Acid Reflux – regurgitation of acid caused by open esophageal sphincter
Body Odor – due to microbial overgrowth
Undigested Food in Stools – your body cannot digest food properly
Meat Aversion – the protein in meat is difficult to digest, but even more so with low stomach acid
Post-Meal Fatigue – your body struggles to digest food and works harder
Full, But Hungry – your body may not absorb nutrients properly, so you’re hungry even when you eat
Chronic Anemia – you get sufficient iron and aren’t losing blood, but you’re still anemic
Food Sensitivities – you can eat an identical meal as someone else, but you get ill.
Causes of Low Stomach Acid
Many things can cause low stomach acid levels and sometimes their combined effects cause health issues. Here are the most common causes a skilled practitioner looks at if you have chronic health issues.
Proton pump inhibitors – doctors prescribe these to alleviate the symptoms of acid reflux, but they lower acid levels, promote microbial overgrowth, and stress the body.
Antibiotic Overuse
Your gut microbiome houses good bacteria important for health. When you take antibiotics, it affects this bacteria too which can lead to inflammation and lowered stomach acid production.
H. Pylori Overgrowth
- Pylori bacteria are part of your microbiome, but without sufficient stomach acid they can grow, unchecked. It can lead to urease production which causes bad breath and belching. It also neutralizes stomach acid which promotes additional bacterial growth.
Stress
Chronic stress affects the parasympathetic nervous system and restricts digestive tract activity.
Poor Diet, Eating Quickly
Additives, preservations, sugars, salt, and grains may cause chronic inflammation, and increased stress hormones. Eating on the go or too quickly stresses the body and does not encourage proper digestion.
Overusing Painkillers
Painkillers such as acetylsalicylic acid (aspirin), acetaminophen (Tylenol), naproxen (Aleve) and ibuprophen (Advil) are fine is small doses, However, NSAID overuse can erode the stomach lining and reduce stomach acid.
Small Intestinal Bacterial Overgrowth (SIBO)
This is a bit of a chicken and the egg discussion. We do not know whether low stomach acid lets bacteria and undigested food into the digestive system, or whether the bacterial overgrowth stresses the body to lower stomach acid levels, but they’re connected.
Aging
Stomach acid levels decrease naturally as you age. After 50, you may need HCL supplements to boost stomach acid levels.
Food Sensitivities
If your body produces an immune response when you eat particular foods, it stresses your body. Common irritants include grains, nuts, and pasteurized dairy.
Self-Tests for Low Stomach Acid
Don’t jump to conclusions if you exhibit any of these symptoms. Start with these 3 self-tests before visiting a practitioner.
Baking Soda – dissolve a small amount of baking soda in water and drink it first thing in the morning. If you do not burp, you may not have sufficient stomach acid.
Betain Hydrochloride – if this supplement produces indigestion or a warm, burning sensation you probably have high stomach acid, not low. Take baking soda and water to neutralize the effect, but do not try this if you have stomach ulcers or are on a long-term NSAID therapy.
Lemon Juice for Heartburn – take a teaspoon of lemon juice when you have heartburn. If you feel better, you probably have low stomach acid.
Seek Assistance
If you suspect you have low stomach acid, the next step is to visit a qualified functional practitioner. They may order a variety of tests such as routine complete blood counts (CBC) and Ferretin test to check for pernicious anemia.
Other possible tests include a comprehensive metabolic panel (CMP) to measure blood glucose levels, electrolyte and fluid balance, and liver and kidney function. A gastro test can help access the acidity levels in your stomach, and a stool analysis offers information on how well your body digests proteins. Finally, they may order x-rays or other images to test for diseases such as osteoporosis with proven links to low stomach acid. Tests such as a CBC and CMP are routine medical tests usually covered through your insurance.
These tests provide a myriad of information important to identify whether you have low stomach acid, the severity of the problem if you do, and how and where it affects your body. Indicators include low chloride, phosphorous or B12 levels, abnormal serum protein and serum globulin levels, high blood urea nitrogen levels, abnormal red blood size, high homocysteine levels, and more.
When one of my patients has symptoms of low stomach acid and two or more indicators from tests, I focus on strategies to improve HCL production
Improving HCL Naturally
The following tips can help you improve stomach acid levels naturally to promote overall health.
Reduce Stress – Eat when relaxed and meditate 10 to 20 minutes twice a day, preferably before breakfast and dinner.
Eat a Whole Food Diet – Steer away from refined sugars, white flour, artificial sweeteners, flavorings and dyes, and preservatives. Don’t eat processed or fast foods or those with genetically modified ingredients. Focus on a plant-based diet and prepare your own meals.
Chew, Chew, Chew – Chew foods thoroughly to stimulate digestive enzymes and to break food down into small particles.
Avoid Cold Water With Food – Icy water slows the production of stomach acid. Drink room temperature or warm water with lemon juice or vinegar before you eat to stimulate HCL production. Gradually increase the lemon juice or vinegar. If it causes a burning sensation, reduce the amount.
Marinate Meat – Marinate meat in high acid substances such as apple cider vinegar, tomato juice, lemon juice, or lime juice. It tenderizes the meat and makes it easier to digest.
Eat Proteins With Veggies – Don’t eat your salad and then your protein. Eat them together for improved HCL production. Spinach, celery, and black olives are especially good HCL stimulants.
Eat Healthy Fat With Protein – Eating healthy fat such as avocado or olive oil with protein stimulates stomach acid and bile.
Use Natural Sweeteners – Avoid processed sugar – use stevia, maple syrup or honey instead.
Spice It Up – Use natural herbs and spices to stimulate HCL, especially black pepper. Quality sea salt stimulates stomach acid production. Check the label if you buy bottled spices. They often have unwanted ingredients.
Sit Upright After Meals – Try not to lie down on the sofa or bed after you eat. You’ll digest food better if your upper body stays upright.
Dandelion Greens & Cabbage Juice – Add dandelion greens to meals and drink freshly -squeezed cabbage juice to increase hydrochloric acid.
Eat Unpasteurized, Salt-Free Sauerkraut – Eat 1/4 to 1/2 cup of unheated sauerkraut with your meals. It balances stomach acids.
Increase Zinc Intake – Zinc is important for stomach acid production. You can increase zinc levels by eating pumpkin seeds, beef, chicken, lamb, turkey, crab, lobster, clams, salmon, yogurt, kefir, cheese, yeast, peanuts, beans, wholegrain cereals, brown rice, and potatoes, if your diet permits them.
Sufficient B Vitamins – B vitamins are important for HCL production. I commonly recommend niacin, thiamine, pyridoxal-5-phosphate (the active form of vitamin B6). You also need sufficient vitamin C, E, and minerals such as magnesium.
Supplementing HCL
Sometimes a patient cannot produce their own HCL or the patient has very low levels. It may be due to prescription drugs or other factors. In this case, I recommend a hydrochloric acid supplement. The idea is to nurture the body so it can begin to produce HCL once again.
The treatment I commonly recommend is betaine HCL and pepsin, because they work well together. Dosage ranges for betaine HCL range between 300 and 500mg per capsule and pepsin 100 to 200mg per capsule.
I suggest two protocols – one for patients who rarely (once a month) or never experience acid reflux, and one for those who have acid reflux regularly.
No Acid Reflux
Always take the betaine HCL mid-meal or at the end of the meal, not before. Take 1 capsule and notice whether you experience a burning sensation like mild heartburn or indigestion. If you do, you’re producing sufficient HCL. If you don’t, you will need to take 2 capsules with your next meal.
Continue to increase the dosage until you discover how much you need. If you find 4 capsules gives you indigestion, take 3 with large meals with protein such as meal, fish, and eggs. Do not reduce the amount if you are consuming a protein shake or bone broth.
Eventually, 3 capsules will cause indigestion as your HCL levels rise. Reduce the capsules to 2, and so on.
Acid Reflux
Always take the betaine HCL mid-meal or at the end of the meal, not before. Do not take antacids or acid reflux medications while taking betaine HCL.
Start by taking 1 capsule to see whether you experience indigestion. If so, you need to increase the dosage with your next meal. Continue to increase the dosage with each meal until you no longer experience indigestion.
Stay with this amount until you notice you have indigestion again. When this happens, reduce your dosage by one capsule during your next meal. Continue this dosage until indigestion reappears, and reduce the dosage during your next meal. You may eventually plateau or eliminate the HCL capsules.
Will I Always Need HCL?
That depends. Your body should produce HCL naturally, so younger and healthier people are more likely to regain optimal production. People with health issues or older individuals may need additional support if they cannot restore their stomach acid production even after following their protocol.
Luckily, many patients can optimize their digestion easily with supplements, and they’re very inexpensive. Others can use them marginally, but either way HCL supplements can improve your quality of life.

Digestion Herbs to the Rescue
Start incorporating ginger, cumin (regular, not black), coriander, fennel and cardamom in your cooking. These spices have powerful digestive benefits that support digestive health.
When you put them all together, something magical occurs. This is an old ancient formula that has been used for thousands of years to reboot digestion. These herbs work together in part by decongesting your bile ducts and improving your production of hydrochloric acid, digestive enzymes and pancreatic enzymes.
This combination of herbs helps build digestive health in multiple ways:
- Increase bile flow
- Increase pancreatic enzyme activity
- Increase small intestine enzyme activity
- Decrease gas and bloating
- Increase fat and sugar metabolism
- Powerful free radical scavengers
- Support optimal weight
- Support a healthy microbiology
- Discourages H. Pylori from adhering to the stomach
- Improves the transit time in the intestines, supporting better elimination
Next, to improve bile flow from your gallbladder and improve your ability to digest fats, incorporate bile-promoting foods such as artichokes, fenugreek, fennel, beets, apples and celery into your diet. Drinking a small number of juiced beets, apples and celery with your meal is a simple way to improve your digestion. Fenugreek tea or fennel tea are other traditional options.
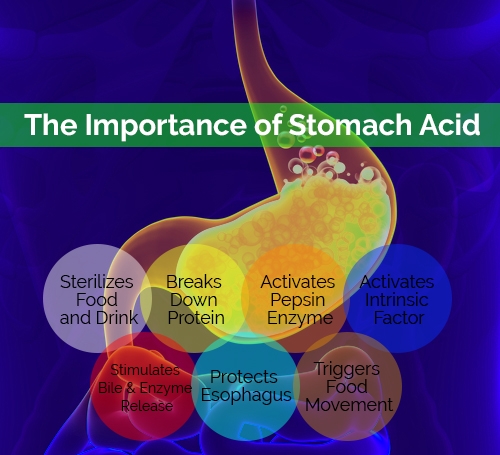
Does Your Bile Need a Reboot?
If you answer yes to one or more of these questions your gallbladder may need support.
- Do you ever get nauseated following meals?
- Do you feel full and heavy after a high fat meal?
- Do you ever get heartburn after a meal?
- Do you ever have sluggish, green or greasy stools?
- Do you have a history of gallbladder problems?
Your bile flow allows you to go to the bathroom. It regulates bowel movement function. It detoxifies you, scrubs your intestinal villi. It allows for emulsifying of fats, for delivering good fats to your brain and your body by getting rid of the bad fats. It buffers the acids from your stomach and without that, digestively, we’re in big trouble.
How to Restore Bile Flow Naturally
Beets are a fantastic food for improving bile flow try to eat one red beat per day for a few weeks to reset bile flow.
It is important to remember that bile is a fantastic detoxifier in the intestine, but it need fiber to assist in the process so eating the whole beat and not juicing the beat is important. As the bile moves thought the small intestine it pics up toxins then the bile attaches to the fiber in the intestine and gets escorted out of the body. If you do not have adequate fiber, then the bile can be reabsorbed back into the circulation to be reused and the toxins get recirculated into your system.
An Apple a Day
Apples are high in malic acid; malic acid has been shown to break up calcium oxalate stones in the kidney and may also help with gallbladder stones. Malic acid has been shown to dilate the bile ducts and aid in bile duct function.
Other foods to support healthy bile and liver function
- Garlic
- Beets
- Celery
- Ginger
- Coconut oil
- Hibiscus
- Apples
- Avocado
- Chicory
- Black radish
- Dandelion
- Berries
- Lemon
- Olive oil
- Ginger
- Mustard greens
- Turnip greens
- Peppermint
- Leafy green
- Cranberries
Has Your Gallbladder Been Removed?
In my practice I see many people who have had their gallbladder removed. This is one of my pet peeves. Conventional medicine does not recognize the importance of the gallbladder to overall health. If a person has symptoms of gallbladder issues the standard of care is “when in doubt take it out.” This practice can have long term consequences that result in further disease and poor health as a direct result of removing the gallbladder. If conventional doctors were taught the importance of the gallbladder and understood how to correct the problem without drugs or surgery a tremendous amount of needless future disease and complications could be avoided.
If you have had your gallbladder removed do not fear, you can supplement with digestive enzymes to support the digestive process. It is not ideal but being aware of the importance of bile acids to your health will help you do the best with an imperfect situation. You will have to take digestive enzymes for life since you no longer can store bile naturally.
Build a Strong Foundation
Proper digestion is the foundation of any functional medicine program. You must have a strong digestive foundation to heal from any disease or condition. Implementing these strategies into your life can have magical results with even the most serious illness but most importantly these practices can prevent future illness and problems from developing in the first place.
*****
Instead of randomly supplementing, try a targeted approach for improved results and less unnecessary products. A skilled practitioner looks at your overall health, performs tests to determine your needs, and recommends what’s best for you.
If you have digestive issues, I would be happy to guide you towards recovery.
Mark A. Scott, D.C., C.N.S., C.F.M.P.