Unraveling the Gut-Parkinson’s Connection: The Intriguing Link between Gut Health and Parkinson’s Disease
Parkinson’s disease (PD) has long been associated with the brain, but emerging research suggests that an unexpected player may have a critical role in its development and progression: the gut. The human gastrointestinal tract is home to trillions of microorganisms collectively known as the gut microbiota, forming a complex ecosystem called the microbiome. Recent studies have shed light on the intriguing relationship between gut health and Parkinson’s disease, revealing a potential avenue for novel therapeutic approaches. In this article, we explore the fascinating connections between Parkinson’s disease and the microbiome, highlighting the impact of gut health on this debilitating neurological disorder.
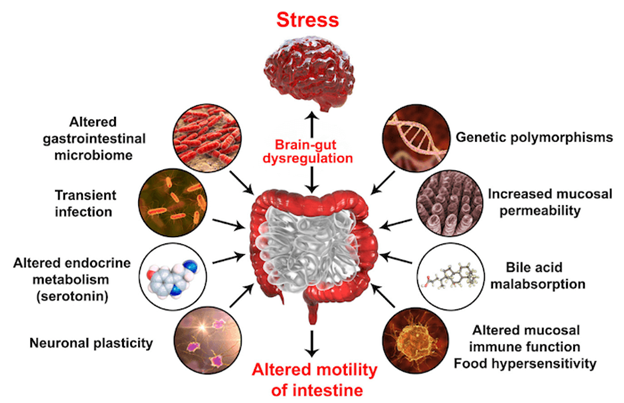
The Gut-Brain Axis: A Bidirectional Communication Highway:

The gut and the brain are intricately connected through a bidirectional communication pathway known as the gut-brain axis. This network involves various pathways, including neural, hormonal, and immunological connections. The gut microbiota plays a crucial role in this axis by influencing the signaling between the gut and the brain.
Gut Microbiota Dysregulation and Parkinson’s Disease:
Recent scientific studies have indicated that individuals with Parkinson’s disease often exhibit alterations in their gut microbiome composition compared to those without the disease. Dysbiosis, an imbalance in the gut microbiota, has been linked to several key features of Parkinson’s disease, including the accumulation of alpha-synuclein protein, the hallmark of this disorder.
Alpha-Synuclein: The Gut’s Connection to Parkinson’s:
Alpha-synuclein is a protein found in the human brain, and its aggregation into clumps called Lewy bodies is a defining characteristic of Parkinson’s disease. Strikingly, evidence suggests that these alpha-synuclein aggregates may originate in the gut before migrating to the brain via the vagus nerve. Research conducted on animal models has demonstrated that gut microbes can promote the misfolding and accumulation of alpha-synuclein, potentially triggering the development of Parkinson’s disease.
Inflammation and the Microbiome-Immune System Axis:
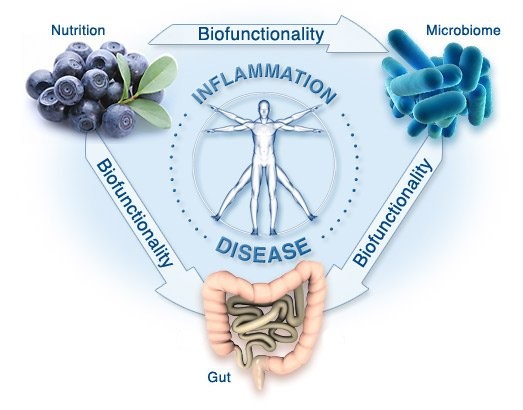
Chronic inflammation is another important factor implicated in Parkinson’s disease. The gut microbiota plays a pivotal role in modulating immune system function and maintaining a balanced inflammatory response. Dysbiosis can disrupt this delicate equilibrium, leading to an increased release of pro-inflammatory molecules. The subsequent inflammation may contribute to the degeneration of dopamine-producing neurons, a hallmark of Parkinson’s disease.
Therapeutic Implications:
Understanding the link between gut health and Parkinson’s disease opens up promising avenues for potential therapies. Researchers are actively exploring interventions that target the gut microbiome to alleviate PD symptoms or slow disease progression. Some strategies being investigated include probiotics, prebiotics, fecal microbiota transplantation (FMT), and dietary modifications. However, it is important to note that these approaches are still in their early stages, and further research is needed to determine their safety and efficacy.
Promoting Gut Health for Overall Well-being:
Maintaining a healthy gut microbiome is essential for overall well-being, regardless of whether someone has Parkinson’s disease or not. Simple lifestyle changes can positively impact gut health, such as consuming a balanced diet rich in fiber, avoiding excessive use of antibiotics, managing stress, and engaging in regular physical activity. Such habits support a diverse and thriving microbiome, potentially benefiting both gut and brain health.
Conclusion:
The relationship between gut health and Parkinson’s disease is a rapidly evolving area of research. While the precise mechanisms linking the gut microbiome to the development and progression of Parkinson’s are still being unraveled, evidence suggests that a disrupted gut ecosystem may contribute to the disease. By investigating the gut-brain axis, researchers hope to identify new therapeutic strategies that can alleviate symptoms and improve the quality.